Northwell Labs to have coronavirus testing capabilities within a week
Northwell Health Labs expects to begin testing for the coronavirus within a week, now that the U.S. Food & Drug Administration has given the green light for outside labs to conduct the COVID-19 tests once appropriately validated.
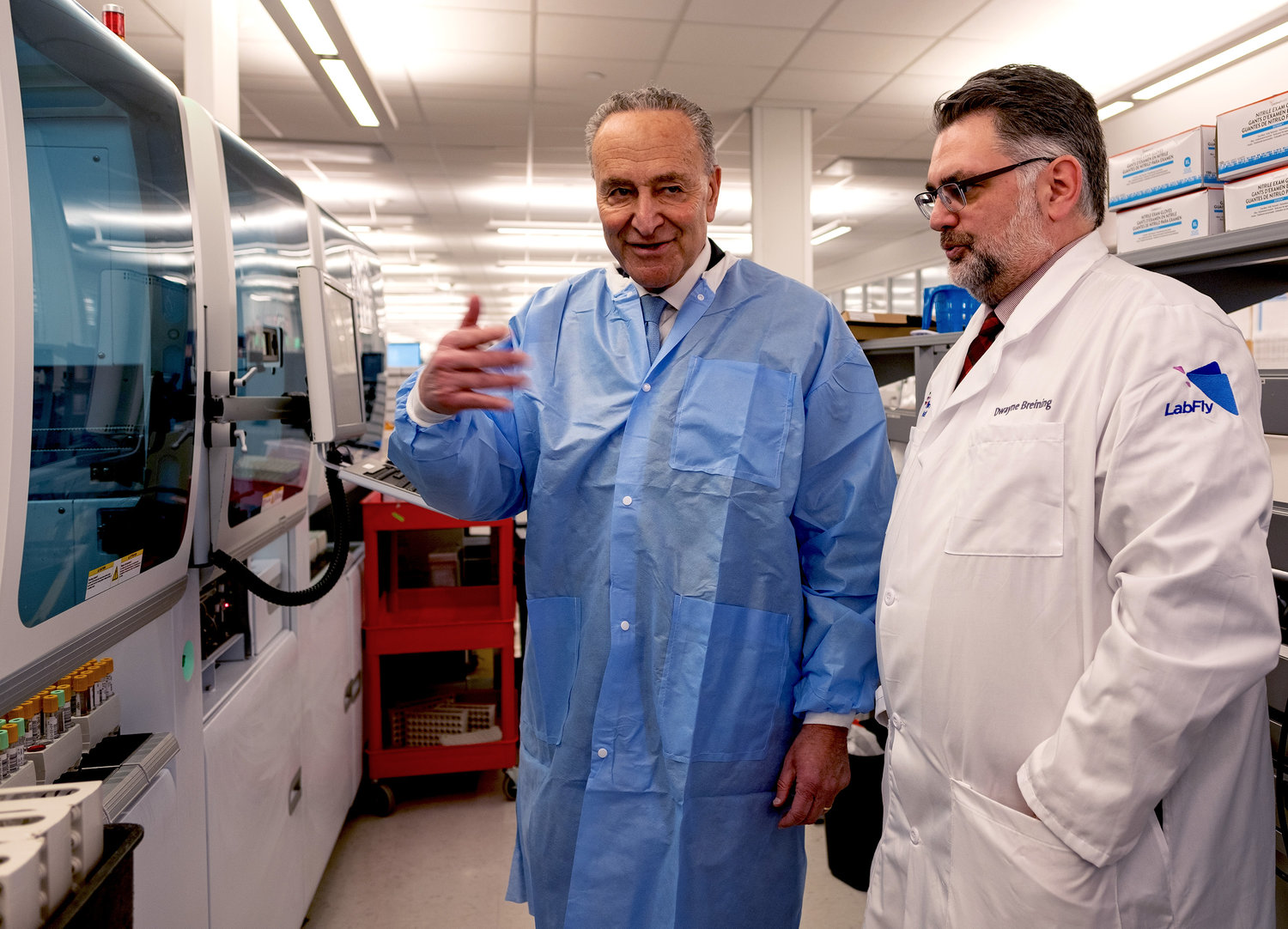
At a news conference today with U. S. Senator Charles Schumer at the 101,000-square foot Core Lab within Northwell’s Center for Advanced Medicine in Lake Success, Dr. Dwayne Breining executive director of laboratory services at Northwell, said manual testing for coronavirus could begin this week, with 75-100 tests processed daily. Once the lab automates the process, it will have the capability to process hundreds and eventually thousands of tests daily, he said.
“Once the process is fully automated, we will have the ability to conduct tests within three-to-four hours of receiving samples at the lab and report the results immediately,” he said.
Prior to this week, all nasopharyngeal swab samples from patients who met the criteria for testing established by the U.S. Centers for Disease Control & Prevention had to be sent to the CDC’s lab in Atlanta for testing. The turnaround time for results was multiple days. To date, Northwell has referred only four samples from suspected cases to the CDC for testing.
“If the virus continues to spread (there is currently only one confirmed case in New York and about 86 nationwide), the ability to have local lab-testing capability is vitally important,” Breining said.
Over the next month the lab is working with test manufacturers to make this testing available within Northwell’s hospitals throughout New York City, Long Island and Westchester County, further expanding the health system’s ability to respond to an epidemic. Those facilities are already doing rapid molecular testing for the seasonal flu using similar technology. “With local labs, you can test quicker and get the results quicker,” Breining added.
The expanded ability to test patients for COVID-19 will greatly enhance Northwell’s ability to manage patients with the potential infection. However, given the limited testing capacity and the CDC’s current recommendations, patients with milder symptoms who do not require hospitalization will not be tested. Such testing is currently reserved for patients who have had contact with someone infected with the virus, or those who are very sick and will require hospitalization.
Over the past six weeks, Northwell invested more than $5 million on coronavirus preparation, including more than $2 million for lab testing and supplies.
Constructed at a cost of $59.6 million and opened in 2019, the Core Lab features North America’s largest Roche Diagnostics automated testing line of its kind and one of the biggest in the world. It currently processes more than 20 million tests annually.
Throughout all of its hospitals and approximately 800 outpatient locations, Northwell continues to maintain a vigilant approach to protecting patients, staff and local communities from the virus. The health system’s clinical protocols are designed to quickly identify potential infectious patients as they enter our facilities, isolate them appropriately, prevent transmission of infections and protect front-line caregivers from potential exposure.
“Northwell is well-prepared to manage the challenges posed by the coronavirus, as evidenced by our response to previous infectious disease outbreaks, including our Anthrax response in 2001, SARS in 2003, swine flu in 2009 and Ebola in 2014,” said Michael Dowling, Northwell Health’s president and CEO. “It’s important for people to remain calm and take practical steps such as routine handwashing to protect against not only the coronavirus but the flu, which has already affected 26 million Americans this season and killed more than 16,000.”
Northwell Health has plans in place for all of its 23 hospitals, including Glen Cove, if people become infected with the coronavirus. Mary Mahoney, Northwell’s vice president of emergency management and clinical preparedness, said that it would increase its isolation capacities in every hospital.
“We thought through what it would take if we had to add an additional 50, 100 or more isolation patients in our hospitals,” Mahoney said. “While this disease does not require a specialized treatment unit, the CDC does require private rooms,” she added. “We would have 30 beds available at Glen Cove Hospital, the equivalent of two hospital wings.”